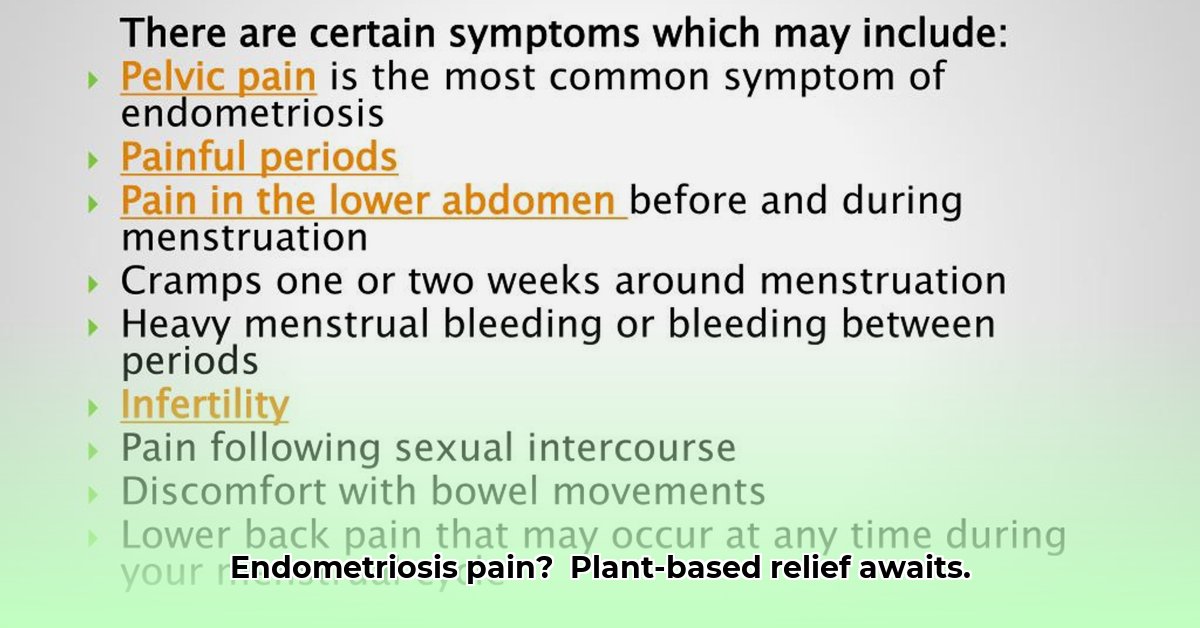
Endometriosis, a condition affecting millions, brings unpredictable pain and disrupts daily life. This guide explores how dietary changes, particularly a plant-based approach, can help manage symptoms, offering actionable steps, evidence-based information, and a personalized path to reclaiming your well-being. For more on plant-based diets and autoimmune conditions, see this helpful guide: Autoimmune diets.
The Promise of Plant-Based Eating for Endometriosis Relief
Living with endometriosis often feels like a constant struggle against chronic pain. A plant-based diet may offer relief by easing symptoms and enhancing overall well-being. Integrating plant-based nutrition with key nutrients offers a proactive approach to managing this challenging condition.
The Food-Endometriosis Connection: Understanding the Impact
Endometriosis involves tissue similar to the uterine lining growing outside the uterus. There’s no cure, but research shows a link between diet and the body’s response, especially concerning inflammation. Diets high in processed foods, red meat, and sugar can worsen symptoms, while plant-based diets rich in fruits, vegetables, and whole grains may reduce inflammation and provide relief.
Plant-Power: A Nutrient-Rich Strategy
A plant-based diet for endometriosis prioritizes nutritious food choices to reduce inflammation and support overall health. It’s about incorporating fruits, vegetables, fiber-rich beans, lentils, and whole grains for sustained energy.
Emphasize these inflammation-fighting nutrients:
- Fiber: Aim for 30-40 grams daily for hormone regulation and digestive health. Sources: oats, beans, lentils, fruits, and vegetables. Fiber binds to estrogen in the digestive tract, aiding its removal from the body, thus helping to balance hormone levels.
- Omega-3 Fatty Acids: Found in flaxseeds, chia seeds, walnuts, and algae-based supplements (for vegans), these can lower inflammation. Omega-3s produce resolvins and protectins, compounds that actively reduce inflammation.
- Magnesium: Crucial for muscle function and relaxation, it eases endometriosis-related cramps. Sources: leafy greens, almonds, pumpkin seeds, and dark chocolate.
- Iron: Replenishing iron stores is important due to potential blood loss during menstruation or endometriosis-related bleeding. Sources: lentils, spinach, tofu, and fortified cereals. Combining iron-rich foods with vitamin C enhances absorption.
Minimize foods that fuel inflammation:
- Red Meat: Limiting intake may reduce endometriosis symptoms due to its inflammatory compounds.
- Processed Foods: High in unhealthy fats, additives, and refined sugars, these can worsen inflammation.
- High-Glycemic Carbohydrates: White bread, sugary cereals, and processed baked goods cause blood sugar spikes and inflammation. Choose complex carbohydrates like brown rice, quinoa, and sweet potatoes.
- Saturated and Trans Fats: Processed foods often contain these unhealthy fats that contribute to inflammation. Opt for olive oil, avocados, and nuts.
- Alcohol: Limit or avoid alcohol due to its potential inflammatory effects and impact on hormone levels.
A quick guide:
| Foods to Prioritize | Foods to Minimize |
|---|---|
| Berries (strawberries, blueberries) | Red meat |
| Leafy greens (spinach, kale) | Processed foods (fast food, snacks) |
| Legumes (beans, lentils) | High-glycemic carbs (white bread, pasta) |
| Whole Grains (quinoa, brown rice) | Saturated/trans fats (fried foods) |
| Nuts and Seeds (flax, almonds) | Refined sugars (soda, candy) |
| Fatty Fish (salmon, mackerel) | Alcohol |
Personalizing Your Plan: Listen to Your Body
Every person is unique. Experiment to discover what works best for you.
Step 1: Food Journal: Record everything you eat, including portion sizes, for at least three weeks.
Step 2: Symptom Tracking: Track pain levels and other symptoms (bloating, fatigue) on a scale of 1 to 10 throughout the day, alongside your food intake.
Step 3: Data Analysis: Review your journal to find patterns. Note the relationship between certain foods and changes in symptom severity.
Step 4: Strategic Elimination & Reintroduction: Eliminate suspected trigger foods one at a time for about two weeks to see if symptoms improve. If symptoms improve, reintroduce the food in small amounts and observe if symptoms return.
Step 5: Adapt and Refine: Adjust your plan based on your observations. Regularly review and adapt your diet for long-term success.
Tackling Real-Life Challenges
Switching to a plant-based diet can be challenging. Here’s how to overcome common obstacles:
- Nutrient Deficiencies: Vegan diets may lack vitamin B12, iron, calcium, and vitamin D. Consult with your doctor or a registered dietitian for supplementation guidance.
- Social Situations: When eating out, choose plant-based options or bring your own dish. Communicate your dietary needs to friends and family.
- Cravings: Use healthy substitutes like fruits, nuts, or seeds to satiate cravings.
The Importance of Professional Guidance
Consult your doctor or a registered dietitian before major dietary changes, especially if you have pre-existing conditions or take medications. A dietitian can offer personalized support and guidance, ensuring the transition is smooth and beneficial.
Plant-based eating for endometriosis is a journey requiring patience, self-awareness, and professional support. The potential benefits—reduced pain, increased energy, and improved health—make it a worthwhile pursuit.
Personalizing Your Endometriosis Diet for Optimal Relief
Key Points:
- Plant-based diets can reduce inflammation to help manage endometriosis symptoms.
- Focus on fiber, omega-3s, magnesium, iron, and Vitamin D.
- Minimize red meat, processed foods, and high-glycemic carbs.
- Recognize individual dietary responses.
- Food and symptom tracking aids in pinpointing triggers.
- Consult a healthcare professional before significant dietary changes.
Understanding the Diet-Endometriosis Connection
Endometriosis is influenced by multiple factors. Diet plays a critical role in managing symptoms and reducing inflammation. Dietary changes can often show noticeable improvements within a few weeks, but consistency is key.
Plant-Based Power: Fueling Your Body for Wellness
Plant-based diets rich in fruits, vegetables, whole grains, and legumes reduce inflammation. Fiber eliminates excess estrogen, and omega-3 fatty acids combat inflammation. A varied plant-based diet ensures you receive vital micronutrients.
Limiting processed foods, red meat, and saturated fats reduces inflammation, potentially easing symptoms. High-glycemic carbohydrates may also exacerbate pain. Moderation is key: be mindful of your choices and portion sizes.
Personalization: A Journey of Self-Discovery
Since endometriosis varies among individuals, personalize your diet through self-monitoring. Keep a detailed food journal for at least three weeks, recording food and drink intake and portion sizes. Rate your pain levels to identify patterns. Identify foods consistently linked to increased pain or discomfort, and consider a structured elimination and reintroduction process with one food item at a time. By making slow, iterative adjustments you can better understand your body’s response to particular food types.
- Why Am I Always Thinking About Food? Your Body and Brain Explain - February 2, 2026
- Healthy Eating Is About Quality, Not Just Calories - February 1, 2026
- Healthy Living Products to Elevate Your Wellness Routine - January 31, 2026