Dealing with unexplained tummy troubles, itchy skin, or even scary allergic reactions? You might be surprised to learn it could be a casein allergy. It’s different from lactose intolerance – it’s a reaction to the *protein* in milk, not just the sugar. This guide will help you understand what a casein allergy is, how to spot it, and, most importantly, how to manage it. We’ll cover everything from symptoms and diagnosis to creating a delicious casein-free diet and long-term strategies to stay healthy and happy. Let’s get you the relief you need!
Allergy to Casein Protein: Finding Relief and Living Well
Are you dealing with an allergy to casein protein? Don’t worry, you’re not alone. Many people have reactions to this milk protein – some mild, others quite serious. Let’s explore what this allergy is all about and how you can manage it, ensuring a better quality of life.
Understanding Casein and Its Impact on Your Body
Casein is a major protein in cow’s milk, comprising about 80% of its protein content along with whey, and a common culprit for allergies. It’s different from lactose intolerance. Lactose intolerance is a problem digesting milk sugar, while a casein allergy is a full-blown immune system response. Your body mistakenly identifies casein as a harmful substance, launching an attack with antibodies that cause various symptoms. It’s important to understand this difference because the solutions are completely different. Could your digestive issues stem from a casein allergy rather than lactose intolerance?
Spotting the Signs: Recognizing a Casein Reaction
The symptoms of a casein allergy are incredibly diverse. Some people get mild tummy troubles like bloating, diarrhea, constipation, or vomiting. Others have skin issues, such as hives, itchy rashes (eczema), or just general itchiness. Nasal congestion, sneezing, a runny nose, and itchy eyes can also occur. Sadly, in some cases, a severe allergic reaction called anaphylaxis can occur. This is a medical emergency and includes trouble breathing, swelling of the lips, tongue, or throat, and a sudden drop in blood pressure. Swift recognition of symptoms is key. If you suspect anaphylaxis, use an epinephrine auto-injector (if prescribed) and seek immediate medical help by calling 911. Did you know that casein allergy symptoms can range from digestive discomfort to severe skin reactions and even respiratory distress?
Getting a Diagnosis: Understanding Allergy Tests
Figuring out if you have a casein allergy usually involves a few steps. Your doctor will want to talk about your symptoms and medical history – providing as much detail as possible to help. They may also conduct skin prick tests or blood tests to check for casein-specific IgE antibodies. These tests look for the immune system’s reaction to casein. A positive skin prick test shows a raised, itchy bump where the skin was pricked with casein. A blood test measures the amount of IgE antibodies to casein in your blood. Another common approach is an elimination diet, under the guidance of a healthcare professional. This means temporarily cutting out all casein from your diet for a few weeks and then reintroducing it to see if symptoms return. This process helps confirm the diagnosis and pinpoints casein as the cause. What diagnostic approach is most effective for confirming a casein allergy, and why is medical supervision important during an elimination diet?
Managing Your Allergy: Strategies for a Casein-Free Life
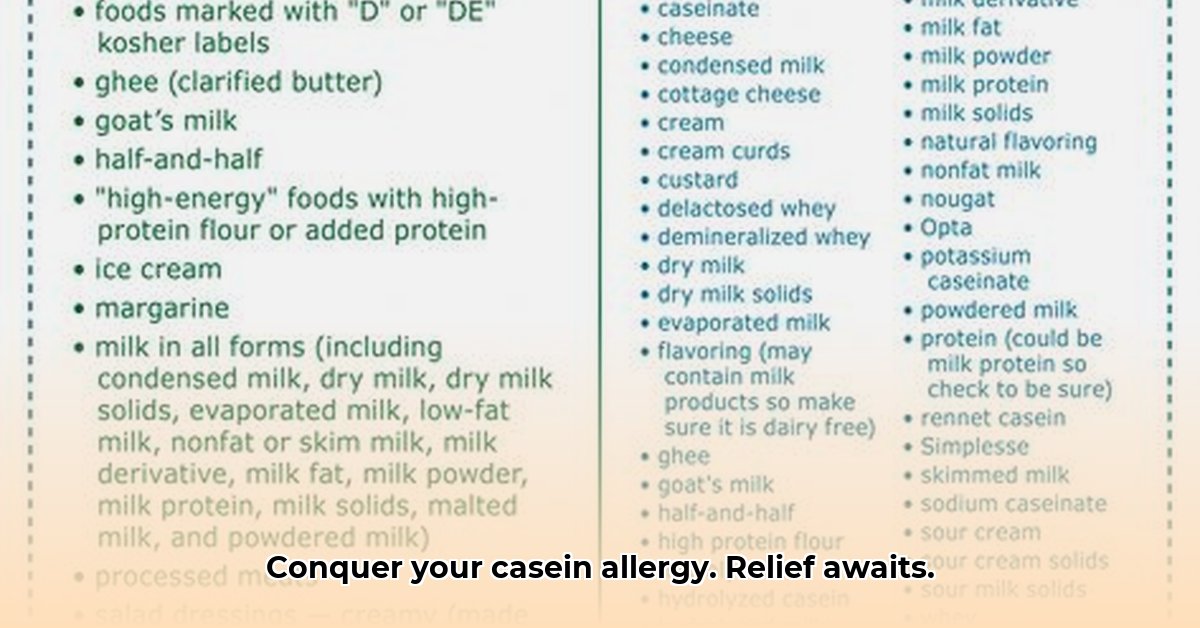
The most effective way to manage a casein allergy is to avoid casein completely. This means becoming a label detective! Carefully read food labels because casein can hide in many processed foods under various names, such as caseinates, whey, and milk solids. Think baked goods, processed meats, sauces, and even some medications. It’s always a good idea to check. When eating out, inform the wait staff about your allergy to avoid cross-contamination and ensure your meal is casein-free. The good news is that many yummy alternatives to dairy exist, including soy milk, almond milk, oat milk, rice milk, coconut milk, cashew milk, and many others! Look for casein-free cheese, yogurt, and ice cream alternatives in the “free-from” aisles of your supermarket. Working with a registered dietitian or nutritionist is a fantastic idea. They can help you create a delicious and nutritious casein-free meal plan tailored to your needs and preferences, ensuring you get all the necessary nutrients. Approximately how many processed foods contain hidden casein, necessitating careful label reading, and what are some common hidden sources of casein?
A Step-by-Step Guide to Casein Avoidance:
- Become a Label Reader: Get into the habit of carefully checking every ingredient list on every food package. Look for “milk,” “casein,” “whey,” “caseinates,” and other milk-derived ingredients.
- Uncover Hidden Casein: Casein can be sneaky! It hides in unexpected places, such as deli meats, nondairy creamers, and even some medications. Learn to recognize it in various disguises.
- Get Expert Help: A registered dietitian or nutritionist can create a personalized diet, offering guidance & support on navigating the complexities of a casein-free lifestyle.
- Find Delicious Substitutes: Explore the wide variety of casein-free milk alternatives (almond, soy, oat, rice, coconut, hemp), vegan cheeses, and dairy-free yogurts.
- Spread the Word: Let your friends, family, coworkers, and anyone who prepares your food know about your allergy. Advocate for yourself and ensure your needs are understood. Safety first!
- Carry Emergency Medication: If you are at risk of anaphylaxis, always carry an epinephrine auto-injector and know how to use it.
What’s New in Research? Hope on the Horizon
While avoiding casein is the main approach now, research continues. Scientists are exploring new therapies, such as oral immunotherapy (OIT) and other forms of immunotherapy (like the Food Allergy Institute’s Tolerance Induction Program). OIT involves gradually introducing tiny amounts of casein into the diet to help the body become less sensitive. This is a promising area, aiming to help the body tolerate food allergens. However, more research is needed to understand its long-term effectiveness, safety, and who it will help best. Researchers are also investigating the role of the gut microbiome in food allergies and potential ways to modify it to prevent or treat allergies. This is an active field of study, and we can hope that future discoveries will expand treatment options. What advancements in immunotherapy offer potential for improving casein allergy management, and what are the limitations and risks associated with these experimental treatments?
Living Well with a Casein Allergy: Long-Term Strategies
Living with a casein allergy long-term involves being proactive and informed. Regular check-ups with your allergist and a registered dietitian are essential. Stay updated on the latest research and new treatments. Consider joining a support group or online community for people with food allergies. Most importantly, remember you’re not alone! There are support groups and communities available to help you connect with others and share experiences.
Casein Allergy vs. Lactose Intolerance: A Quick Comparison
| Feature | Casein Allergy | Lactose Intolerance |
|---|---|---|
| Cause | Immune system reaction to casein protein | Inability to digest lactose (milk sugar) |
| Symptoms | Wide range; from mild to severe (anaphylaxis possible) | Usually gastrointestinal (gas, bloating, diarrhea) |
| Treatment | Complete casein avoidance | Lactose reduction, avoidance or enzyme supplements |
| Severity | Can be life-threatening | Rarely life-threatening |
| Diagnosis | Allergy testing (skin prick, blood test, elimination diet) | Hydrogen breath test, lactose tolerance test, stool acidity test |
Important Note: This information is for educational purposes only and isn’t a substitute for professional medical advice. Always consult with a healthcare professional for diagnosis and treatment.
How to Manage Casein Allergy Long Term for Infants
Key Takeaways:
- Casein allergy, a type of cow’s milk protein allergy (CMPA), affects many infants, causing various symptoms from mild discomfort to severe reactions. The prevalence of CMPA is estimated to be between 2% and 7% in infants.
- Early diagnosis is crucial, often involving a combination of clinical assessment, allergy testing, and a trial elimination diet.
- How to manage casein allergy long term for infants involves a multifaceted approach including strict dietary avoidance, careful formula selection, and close monitoring.
- Many children outgrow casein allergy by age 3-5, but ongoing monitoring for related conditions is vital.
- Gradual reintroduction of casein under medical supervision is possible as the child gets older.
- Support from healthcare professionals, including pediatricians and allergists, is essential throughout the process.
Understanding Casein Allergy in Infants
Casein, a major protein in cow’s milk, can trigger allergic reactions in some infants. These reactions vary widely – from mild digestive upset (colic, fussiness, diarrhea, vomiting, reflux) to more serious issues like eczema, hives, angioedema (swelling), respiratory problems (wheezing, coughing), or even life-threatening anaphylaxis. In severe cases, CMPA can lead to failure to thrive. Do you know the signs your little one might be showing? It’s important to be aware and seek medical advice if you suspect an allergy. What percentage of infants experience cow’s milk protein allergy (CMPA), including casein allergy, and what are the potential long-
- Why Am I Always Thinking About Food? Your Body and Brain Explain - February 2, 2026
- Healthy Eating Is About Quality, Not Just Calories - February 1, 2026
- Healthy Living Products to Elevate Your Wellness Routine - January 31, 2026