Knee injuries, such as ACL (anterior cruciate ligament) and MCL (medial collateral ligament) tears, can be daunting. Understanding the injury and recovery process is crucial for a successful return to your active lifestyle. This article provides a clear breakdown of ACL, MCL, and meniscus tears, covering causes, diagnosis, and treatment options. Whether you’re experiencing initial symptoms or navigating recovery, this guide will empower you to make informed decisions about your healing journey. For more in-depth information, check out this helpful resource on knee ligament injuries.
Understanding Knee Ligament Injuries and Available Treatments
Knee injuries, particularly ACL and MCL tears, can significantly hinder your active lifestyle. These ligaments are crucial for knee stability, and a tear can be a major setback. This guide provides essential information to help you recover quickly and safely. Are you experiencing pain or instability after a knee injury?
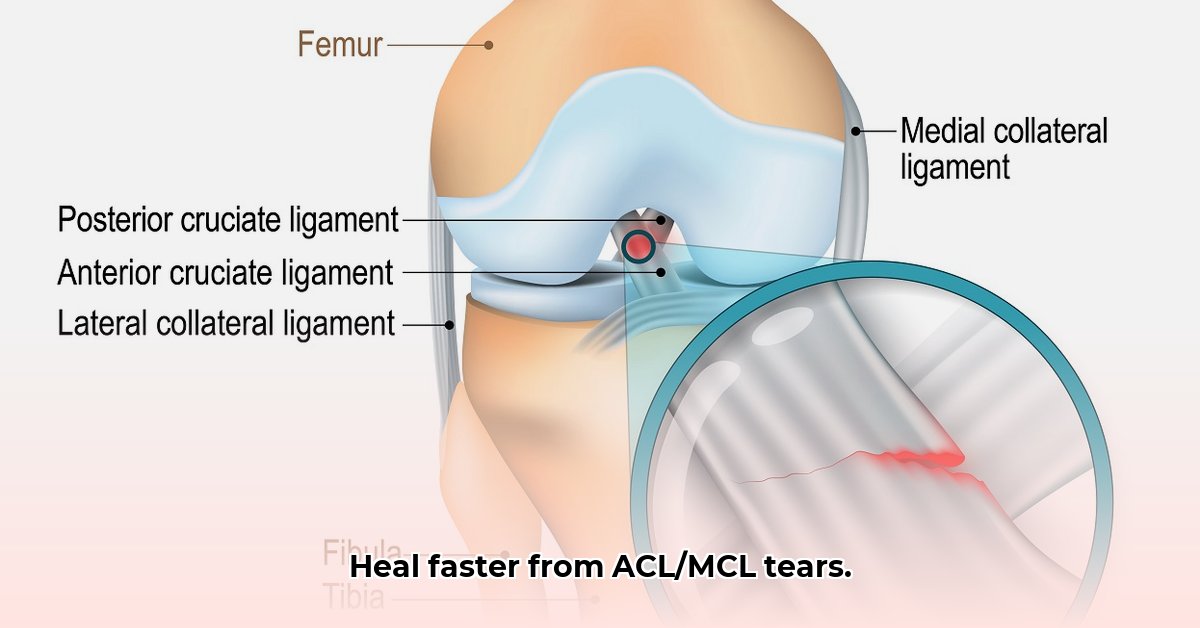
Decoding Your Knee’s Support System
Your knee’s intricate design relies on ligaments like the ACL and MCL for stability. Imagine them as strong ropes holding the bones together. The ACL, located in the center of the knee, acts as the knee’s primary stabilizer, preventing the tibia (shinbone) from sliding forward on the femur (thighbone). The MCL, running along the inner side of the knee, reinforces the joint against excessive inward movement. Damage to either ligament can cause pain, instability, and swelling. What level of knee instability are you currently experiencing?
An ACL tear often presents with a distinct “pop” followed by rapid swelling (effusion) and a feeling of instability, particularly during activities involving pivoting or twisting. An MCL injury, conversely, usually manifests as pain and tenderness on the inner knee, with potential instability during bending or straightening. Bruising may also be present with an MCL tear. These differing symptoms aid doctors in diagnosis, which may require further testing.
Diagnosis: Confirming the Issue and Understanding Severity
Accurate diagnosis is the first step to recovery. Your doctor will conduct a physical exam to assess your knee’s range of motion, stability, and swelling, and to pinpoint the source of pain. Specific tests, such as the Lachman test (for ACL) and valgus stress test (for MCL), will be performed to assess ligament integrity.
Imaging tests, such as X-rays and MRIs, may be ordered. X-rays rule out fractures or other bone abnormalities. An MRI provides a detailed view of your ligaments, allowing for precise assessment of damage extent, from minor sprains (Grade 1) to partial tears (Grade 2) to complete ruptures (Grade 3). Early diagnosis sets the stage for effective treatment.
Treatment Options: Surgical and Non-Surgical Approaches
Treatment approaches vary based on injury severity, activity level, and overall health. Minor ACL or MCL sprains (Grade 1) can often heal with conservative treatment. RICE (Rest, Ice, Compression, Elevation) is a common first step. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help manage pain and inflammation. Physical therapy is typically recommended soon after the injury to guide the healing process and restore function.
However, complete ACL tears (Grade 3) often require surgery, especially for athletes and active individuals seeking to return to high-demand activities. Severe MCL tears (Grade 3) may also warrant surgical intervention, though less commonly, particularly if associated with instability or other ligamentous injuries. Minimally invasive techniques like arthroscopy can lead to smaller scars and faster recovery times. ACL reconstruction involves replacing the torn ligament with a graft, often using a hamstring tendon, patellar tendon, or a donor allograft. The goal of surgery is to repair the torn ligament and restore stability.
Rehabilitation: Rebuilding Your Knee After Acute Injury
Recovery from ACL or MCL surgery, or a severe non-surgical injury, requires a comprehensive rehabilitation program. Physical therapy is like rebuilding your knee, strengthening it, and restoring proper function. A physical therapist will design a customized program tailored to your specific needs and goals.
Rehabilitation Phases:
- Phase 1 (Weeks 1-4): Focuses on pain management, reducing swelling, regaining initial range of motion, and quadriceps activation. Crutches or a brace may be used, along with gentle exercises like ankle pumps, quad sets, and heel slides.
- Phase 2 (Weeks 5-12): Gradually increase range of motion (aiming for full extension and flexion), begin progressive strengthening exercises (e.g., leg presses, hamstring curls, calf raises), and improve balance and proprioception (awareness of joint position in space).
- Phase 3 (Weeks 13 onwards): Advanced exercises build strength, endurance, and agility, progressing toward a return to sport-specific activities. Examples include jogging, jumping, cutting, and pivoting.
It’s essential to listen to your body, adhere to your physical therapist’s guidance, and maintain patience. Progress is not always linear, and setbacks can occur. Open communication with your physical therapist is crucial.
Sample Rehab Schedule:
| Phase | Timeframe | Focus | Examples of Exercises |
|---|---|---|---|
| Phase 1 | Weeks 1-4 | Pain management, range of motion | Ankle pumps, quad sets, heel slides, straight leg raises (with brace if prescribed), gentle hamstring stretches |
| Phase 2 | Weeks 5-12 | Strength building, balance, coordination | Leg presses, hamstring curls, calf raises, balance exercises (single leg stance), stationary cycling |
| Phase 3 | Weeks 13+ | Functional training, return to activity | Jogging, agility drills (cone drills, shuttle runs), plyometrics (jump squats, box jumps), sport-specific drills |
Long-Term Outcomes and Potential Complications for Knee Ligament Injuries
Recovery times vary based on injury severity, age, commitment to rehabilitation, and individual healing rates. Celebrate progress and be patient. Potential complications, though rare, include infection, persistent pain, stiffness (arthrofibrosis), re-tear of the ligament, development of osteoarthritis, or ongoing instability. With proper care and diligent rehab, most individuals achieve full recovery and return to previous activity levels. Full return to sports typically takes 6-9 months after ACL reconstruction.
Frequently Asked Questions About Knee Ligament Injuries
-
Q: How long will my recovery take? A: Recovery times vary significantly depending on the severity of the injury and the treatment approach. Consult your doctor and physical therapist for a personalized estimate. What are your specific recovery goals? Clear communication with your medical team is essential.
-
Q: Are there long-term effects I should be aware of? A: Most individuals recover fully, but some may experience mild arthritis, persistent pain, or a slight decrease in knee stability. Adhering to your rehabilitation program and maintaining a healthy lifestyle can minimize these risks.
-
Q: Can I prevent future knee injuries? A: Yes! Regular exercise focusing on strength and flexibility, proper stretching, maintaining a healthy weight, using good technique during sports (including proper landing mechanics), and wearing supportive footwear can help. Neuromuscular training programs, which focus on improving muscle activation patterns and joint control, can also be beneficial. What steps are you taking to prevent re-injury?
Your healthcare team is your ally. Don’t hesitate to ask questions for a successful recovery.
Deciding Between ACL Surgery and Physical Therapy for a Grade 2 MCL Tear
Key Takeaways:
- Grade 1 MCL tears typically heal with rest and physical therapy.
- Grade 3 MCL tears often require surgery, especially when combined with other ligament injuries.
- Grade 2 MCL tears present a complex decision-making process, requiring careful consideration of individual factors.
- ACL tears usually need surgery for active individuals seeking to return to pre-injury activity levels.
- A thorough medical evaluation, including physical examination and MRI, is critical.
- Rehabilitation is key regardless of treatment choice.
Understanding MCL and ACL Function
Your knee’s stability relies on the ACL and MCL. An MCL tear disrupts the knee’s mechanics and can lead to instability. The MCL, a strong ligament on the inner side of the knee, prevents excessive sideways movement (valgus stress). The ACL, located inside the joint, prevents the shinbone from sliding forward (anterior translation) and provides rotational stability. Both can be injured during sports or falls.
The Grade 2 Dilemma: Non-Operative vs. Operative Knee Treatment
A grade 2 MCL tear involves stretching or partial tearing of the ligament. Unlike a grade 1 tear, it causes more pain and instability. Grade 3 tears often need surgery. The decision for a grade 2 tear depends on your age, activity level, tear severity (as visualized on MRI), presence of other injuries (like ACL or meniscus tears), and overall functional goals. It’s a personalized decision made in consultation with your orthopedic surgeon.
When Physical Therapy May Suffice for Knee Stability
Conservative treatment, including physical therapy, may be the initial approach for a grade 2 MCL tear. The focus is on pain management, reducing inflammation (RICE), and restoring stability and function. Bracing (hinged knee brace) is commonly used to protect the healing ligament. Physical therapy includes strengthening exercises for the surrounding muscles (quadriceps, hamstrings, calf muscles) and improving range of motion.
The main goal with a grade 2 MCL tear is regaining stability and preventing chronic problems. Progress is carefully monitored. If improvement isn’t seen after a period
- Why Am I Always Thinking About Food? Your Body and Brain Explain - February 2, 2026
- Healthy Eating Is About Quality, Not Just Calories - February 1, 2026
- Healthy Living Products to Elevate Your Wellness Routine - January 31, 2026